How Common Is Insulin Resistance in Society?
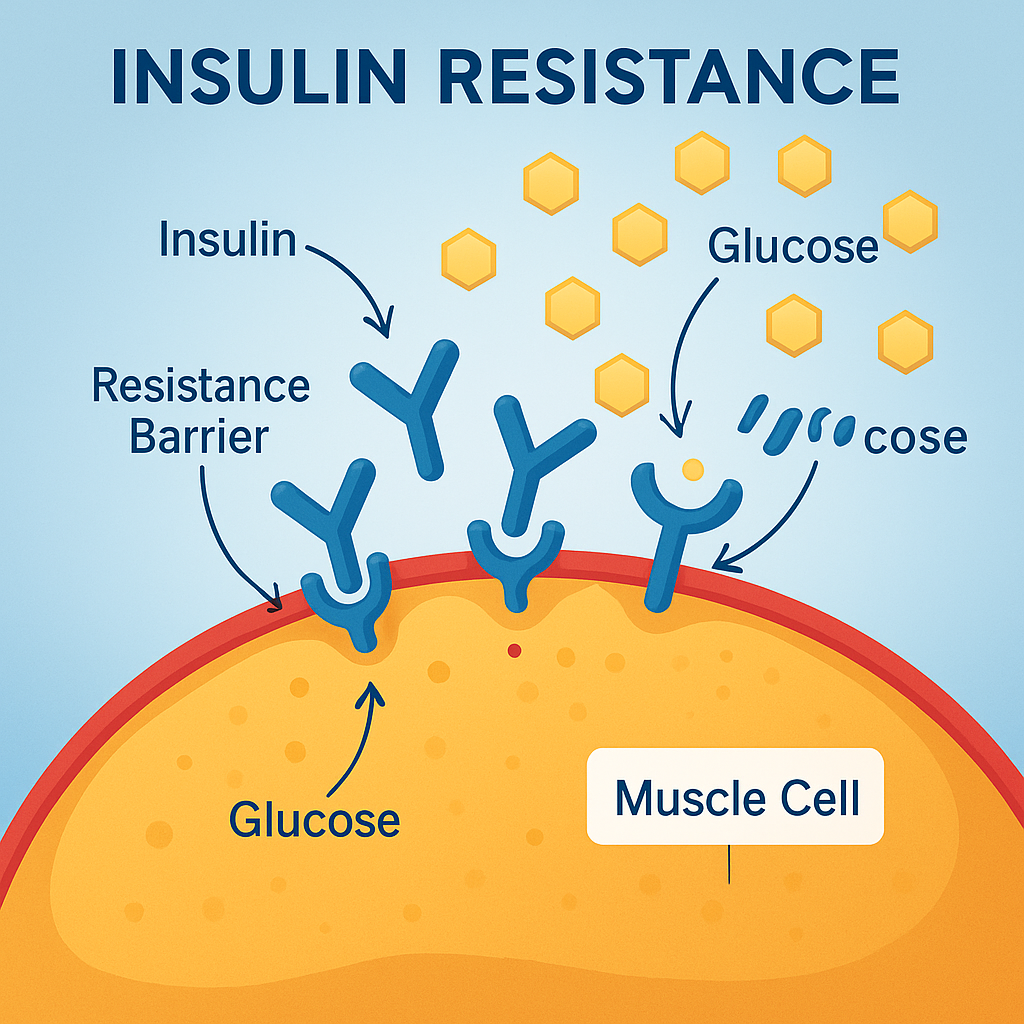
Insulin resistance is often called the “silent precursor” to type 2 diabetes, but it’s far more common—and dangerous—than many people realize. This metabolic condition occurs when your body’s cells no longer respond effectively to insulin, a hormone that helps move glucose from the bloodstream into cells for energy.
At Sheen Vein (Aesthetics and Functional Medicine) in St. Louis, we see insulin resistance frequently—not just in people with diabetes, but in patients struggling with fatigue, weight gain, hormonal imbalances, and cardiovascular risk factors. The surprising truth is that insulin resistance is now affecting more than half of U.S. adults—and many don’t even know they have it.
The Scope of the Problem
According to research from the Centers for Disease Control and Prevention (CDC) and other major studies:
- Over 88 million U.S. adults (more than 1 in 3) have prediabetes, a condition strongly linked to insulin resistance.
- Estimates suggest 50–70% of adults may have some degree of insulin resistance, even if their fasting blood sugar is normal.
- Alarmingly, insulin resistance is rising rapidly among teenagers and young adults due to poor diet, inactivity, and obesity.
Because early insulin resistance often causes no obvious symptoms, it can go undetected for years—until it progresses to type 2 diabetes or causes other health issues.
Why Insulin Resistance Is So Common
The modern lifestyle is a perfect storm for developing insulin resistance. Factors include:
- High-Sugar, Processed Diets
Frequent intake of refined carbohydrates (white bread, pastries, sugary drinks) causes repeated spikes in blood sugar and insulin. Over time, cells become less responsive to insulin’s signal. - Sedentary Living
Physical inactivity means less muscle glucose uptake, forcing the body to produce more insulin to keep blood sugar under control. - Excess Weight, Especially Around the Midsection
Visceral fat (fat stored around the organs) is metabolically active and produces inflammatory chemicals that worsen insulin resistance. - Chronic Stress
Elevated cortisol from stress can raise blood sugar and promote abdominal fat storage. - Poor Sleep
Even short-term sleep deprivation can increase insulin resistance, impairing the body’s ability to regulate glucose.
Hidden Consequences Beyond Diabetes
While most people associate insulin resistance with type 2 diabetes, its effects extend far beyond blood sugar control. It is a major driver of:
- Heart disease – Insulin resistance contributes to high blood pressure, abnormal cholesterol, and vascular inflammation.
- Non-alcoholic fatty liver disease (NAFLD) – Excess glucose is converted to fat in the liver, impairing function.
- Polycystic ovary syndrome (PCOS) – Insulin resistance disrupts hormone balance, affecting fertility and menstrual cycles.
- Cognitive decline – Research suggests insulin resistance increases Alzheimer’s risk (“type 3 diabetes” theory).
- Chronic fatigue and weight gain – Poor glucose utilization leaves cells energy-deprived, even with high calorie intake.
Why So Many Cases Go Undiagnosed
Traditional screening often relies on fasting blood glucose alone. But blood sugar can remain normal for years even when insulin levels are elevated. That means many people with insulin resistance are told their labs are “fine” while the condition quietly progresses.
Better testing includes:
- Fasting insulin – Elevated levels indicate the pancreas is overworking to maintain blood sugar.
- HOMA-IR score – A calculation from fasting glucose and insulin that estimates insulin sensitivity.
- Hemoglobin A1c – Reflects average blood sugar over the past 2–3 months.
Reversing the Trend
The good news: insulin resistance is highly reversible, especially in its early stages. At our St. Louis functional medicine clinic, we take a root-cause approach to improving insulin sensitivity. This may include:
- Dietary changes: Focus on whole, unprocessed foods, high-quality protein, healthy fats, and fiber-rich vegetables.
- Regular exercise: Strength training and interval training increase muscle glucose uptake.
- Weight loss: Even a 5–10% reduction in body weight can significantly improve insulin sensitivity.
- Sleep optimization: Prioritizing 7–9 hours of quality rest each night.
- Stress reduction: Techniques like meditation, deep breathing, or yoga lower cortisol and stabilize blood sugar.
In some cases, targeted supplementation—such as magnesium, berberine, or alpha-lipoic acid—can help support insulin sensitivity, but we always tailor these recommendations to the individual.
The Takeaway
Insulin resistance isn’t rare—it’s a modern epidemic affecting up to two-thirds of adults, many of whom have no idea they’re at risk. Left unchecked, it sets the stage for diabetes, heart disease, hormonal issues, and more.
The earlier it’s detected, the easier it is to reverse. If you have risk factors such as belly fat, high blood pressure, abnormal cholesterol, or a family history of diabetes, it’s worth getting evaluated for insulin resistance now—not years from now when complications appear.
Ready to find out where you stand?
Our team at Sheen Vein (Aesthetics and Functional Medicine) offers advanced testing and personalized plans to restore insulin sensitivity and protect your long-term health.
Learn more about our Functional Medicine services »
Schedule your consultation today »