Why Insulin Resistance Prevents Weight Loss — And How to Overcome It
Understanding Insulin and Its Role in the Body
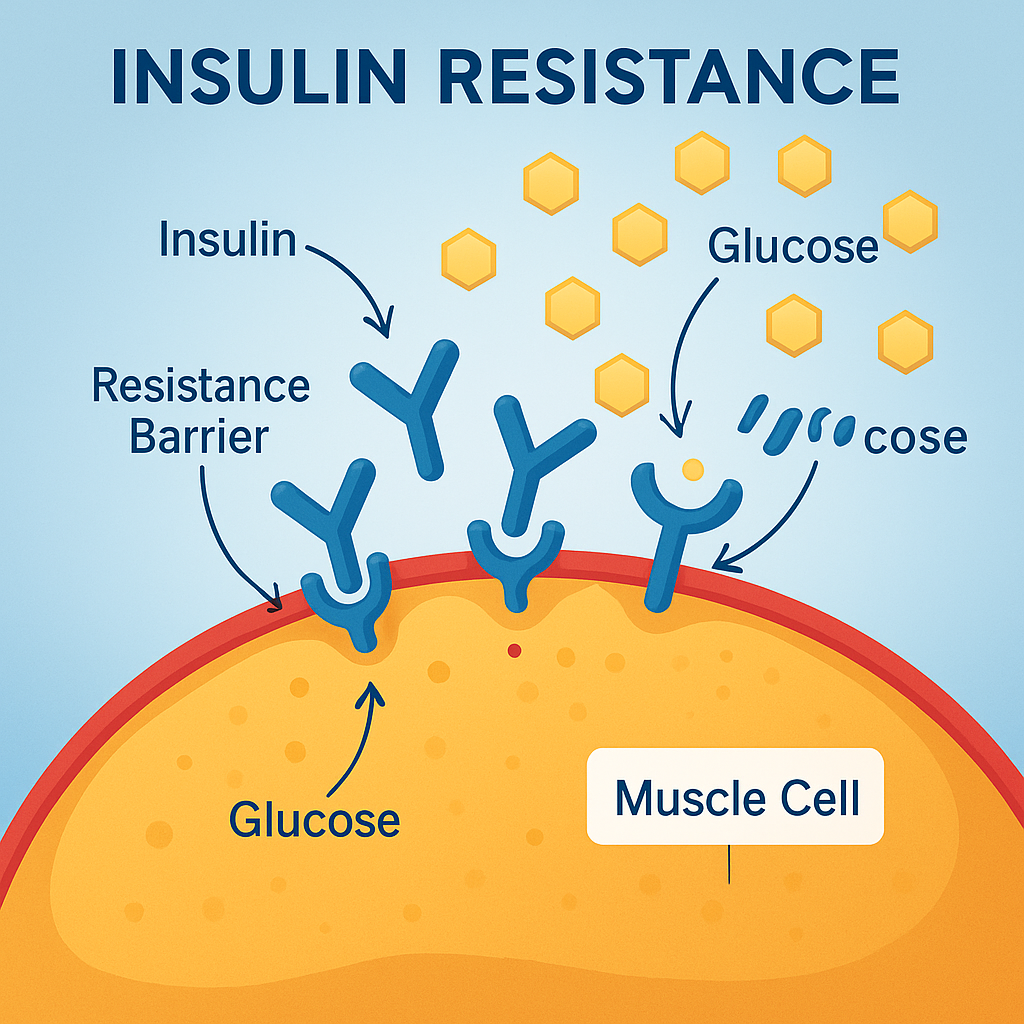
Insulin is a hormone produced by the pancreas that acts like a “key,” allowing glucose (sugar) from your bloodstream to enter your cells for energy or storage. When you eat carbohydrates, your blood sugar rises, and insulin is released to help store that energy for later use.
In a healthy metabolism, insulin levels rise and fall throughout the day in response to food intake. But in insulin resistance, your cells stop responding properly to insulin’s signal. As a result, the pancreas produces even more insulin to try to get the job done. Over time, both insulin and blood sugar remain elevated, setting the stage for weight gain, type 2 diabetes, and other metabolic issues.
What Is Insulin Resistance?
Insulin resistance is a state where your body’s cells — particularly in the liver, muscles, and fat — become less sensitive to insulin’s effects. This means:
- More insulin is needed to maintain normal blood sugar
- Blood sugar can start to rise despite high insulin
- Excess glucose gets stored as fat rather than burned for energy
Insulin resistance can develop gradually, often without obvious symptoms at first, but it has a profound effect on your ability to lose weight.
Why Insulin Resistance Blocks Weight Loss
If you’re struggling to lose weight despite eating less and exercising, insulin resistance may be the hidden culprit. Here’s why:
1. High Insulin Locks Fat in Storage Mode
Insulin is sometimes called the “fat storage hormone.” When insulin levels are high, your body prioritizes storing energy rather than burning it. Even if you’re eating fewer calories, elevated insulin signals your fat cells to hold on to their contents.
2. Sugar and Carb Cravings
Insulin resistance can lead to rapid swings in blood sugar. When blood sugar crashes, your brain signals you to eat more quick energy foods — usually refined carbs or sweets — perpetuating the cycle.
3. Hormonal Disruption
High insulin can disrupt other hormones involved in metabolism, such as leptin (the “fullness” hormone) and ghrelin (the “hunger” hormone), making it harder to control appetite naturally.
4. Reduced Energy for Exercise
Because your cells aren’t using glucose efficiently, you may feel fatigued, making it harder to stay active or exercise at a high intensity.
5. Increased Inflammation
Insulin resistance often occurs alongside chronic low-grade inflammation, which can impair mitochondrial function and slow metabolic rate.
The Common Causes of Insulin Resistance
Several factors can drive insulin resistance:
- Poor diet — Excess sugar, refined carbohydrates, and processed foods
- Sedentary lifestyle — Lack of muscle activity reduces glucose uptake
- Chronic stress — Elevated cortisol can worsen insulin resistance
- Sleep deprivation — Even a few nights of poor sleep can impair insulin sensitivity
- Visceral fat — Fat stored around the organs is metabolically active and promotes inflammation
- Hormonal imbalances — PCOS, low testosterone, and thyroid dysfunction can contribute
How to Know If You Have Insulin Resistance
You can’t always tell by looking at someone, but common signs and risk factors include:
- Difficulty losing weight, especially around the midsection
- Sugar cravings or “hangry” episodes
- Fatigue after meals
- Darkened patches of skin (acanthosis nigricans)
- Elevated triglycerides and low HDL cholesterol
- Family history of type 2 diabetes
Lab tests can confirm insulin resistance, including:
- Fasting insulin
- Fasting glucose
- Hemoglobin A1c
- HOMA-IR score (calculated from fasting glucose and insulin)
The Functional Medicine Approach to Reversing Insulin Resistance
At Sheen Vein (Aesthetics and Functional Medicine) in St. Louis, we address insulin resistance by targeting the root causes and helping the body restore proper insulin sensitivity.
1. Nutrition Reset
We focus on reducing processed carbohydrates and sugars while emphasizing:
- High-quality protein at each meal to stabilize blood sugar
- Healthy fats (avocados, olive oil, nuts, fatty fish) to improve satiety
- Fiber-rich vegetables to slow glucose absorption
- Low-glycemic fruits in moderation
We may recommend a low-carb, whole-foods approach or intermittent fasting for some patients, always personalized to their health status.
2. Movement and Resistance Training
Muscle tissue is a major site of glucose disposal. Resistance training and daily movement improve insulin sensitivity and help shift your body from fat storage to fat burning.
3. Stress Reduction
Chronic stress keeps cortisol — and blood sugar — elevated. We incorporate stress management strategies (see our blog on Stress Management Techniques) such as deep breathing, mindfulness, and gentle exercise.
4. Sleep Optimization
We aim for 7–9 hours of quality sleep per night, as sleep deprivation can reduce insulin sensitivity by up to 30% in just a few days.
5. Targeted Supplementation
Certain nutrients can improve insulin signaling, such as:
- Magnesium
- Chromium
- Alpha-lipoic acid
- Omega-3 fatty acids
- Berberine (a plant extract with insulin-sensitizing properties)
6. Addressing Hormonal Imbalances
For patients with PCOS, low testosterone, or thyroid dysfunction, we create a plan to optimize hormone balance, which can significantly improve insulin sensitivity.
A Patient Success Story
A 46-year-old woman came to our clinic frustrated by years of unsuccessful dieting. She was 40 pounds overweight, had sugar cravings, and felt exhausted after meals. Her labs revealed high fasting insulin and borderline high A1c.
We developed a program combining a lower-carb, anti-inflammatory diet, twice-weekly strength training, magnesium supplementation, and stress-reduction practices. Within three months, she lost 18 pounds, her cravings disappeared, and her energy dramatically improved. By six months, her fasting insulin dropped into the normal range.
The Long-Term Benefits of Reversing Insulin Resistance
Beyond weight loss, improving insulin sensitivity reduces your risk of:
- Type 2 diabetes
- Heart disease
- Stroke
- Fatty liver disease
- Certain cancers
It also boosts energy, mood, and cognitive function — helping you feel better overall.
The Bottom Line
Insulin resistance is one of the most common — and overlooked — reasons people struggle to lose weight. When your cells can’t respond properly to insulin, your body stays in fat storage mode, making weight loss an uphill battle.
The good news: insulin resistance is reversible with the right strategies. By addressing nutrition, movement, sleep, stress, and underlying hormonal imbalances, you can reset your metabolism, burn fat more efficiently, and improve your overall health.
At Sheen Vein (Aesthetics and Functional Medicine), we offer in-depth testing and personalized plans to help you overcome insulin resistance and achieve lasting results. We also provide telemedicine services for patients beyond the St. Louis area.
Internal Link Opportunities:
- Link “stress management strategies” to Stress Management Techniques.
- Link “hormonal imbalances” to How Low Testosterone Can Affect Men and Women.
- Link “gut health” to Fixing Gut Dysbiosis to Help Autoimmune Issues.