How Mitochondrial Dysfunction Causes Chronic Fatigue
How Mitochondrial Dysfunction Causes Chronic Fatigue
We’ve all experienced days of feeling run-down after poor sleep, illness, or stress. But for many people, fatigue isn’t just an occasional issue—it’s a constant companion that makes even simple tasks feel overwhelming. When fatigue becomes chronic, it can’t always be explained by lifestyle alone. One of the root causes we evaluate at Sheen Vein & Cosmetics in St. Louis is mitochondrial dysfunction.
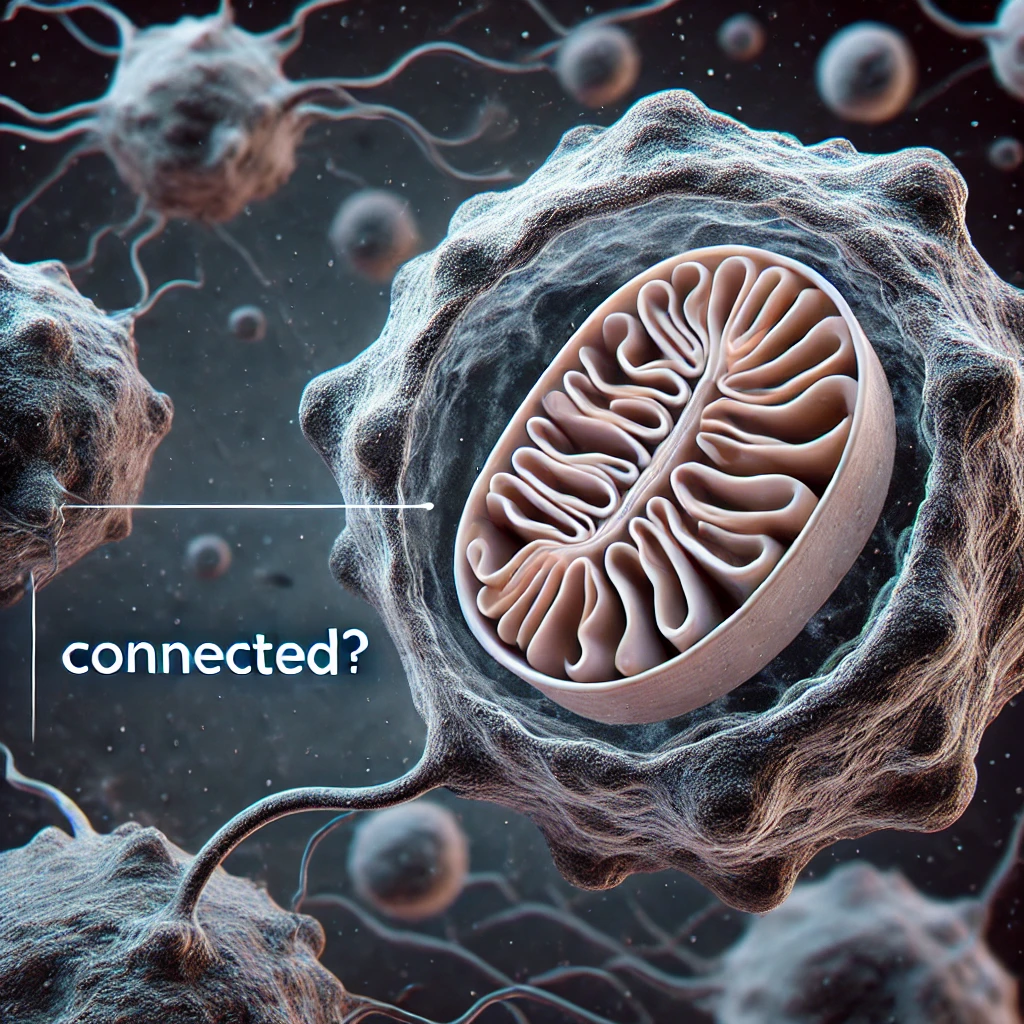
Your mitochondria are often called the “powerhouses” of your cells. They’re responsible for generating the energy your body needs to function. When mitochondria aren’t working properly, energy production drops, and the result is often deep, persistent fatigue that doesn’t improve with rest.
The Role of Mitochondria in Energy Production
To understand why mitochondrial dysfunction can lead to chronic fatigue, it helps to know what mitochondria do. Inside each cell, mitochondria convert oxygen and nutrients from food into ATP (adenosine triphosphate)—the molecule that powers nearly every process in your body.
Whether you’re thinking, exercising, digesting food, or simply breathing, ATP fuels it. Healthy mitochondria keep this energy production steady. But if mitochondria become damaged or inefficient, your body produces less ATP, leaving you feeling tired, foggy, and drained.
What Causes Mitochondrial Dysfunction?
Mitochondrial health depends on a delicate balance. Several factors can interfere with their ability to generate energy:
- Oxidative Stress
Free radicals, often from poor diet, environmental toxins, or chronic inflammation, damage mitochondrial membranes and DNA. Without repair, this leads to decreased ATP output. - Nutrient Deficiencies
Vitamins and minerals such as B vitamins, magnesium, and CoQ10 are essential cofactors for mitochondrial enzymes. Without them, the energy cycle slows down. - Chronic Infections and Immune Activation
Viral or bacterial infections can trigger ongoing inflammation, which impairs mitochondrial efficiency and diverts energy toward immune defense instead of daily function. - Hormonal Imbalances
Thyroid hormones and cortisol directly influence mitochondrial energy output. Low thyroid function, adrenal dysfunction, or low testosterone can all contribute to fatigue. - Toxin Exposure
Heavy metals, pesticides, mold toxins, and pollutants can accumulate in the body and disrupt mitochondrial enzymes, further lowering ATP production.
How Mitochondrial Dysfunction Leads to Chronic Fatigue
When mitochondria cannot produce enough ATP, the effects ripple through the body:
- Low physical energy – Exercise becomes exhausting, and recovery takes longer.
- Brain fog – The brain consumes massive amounts of ATP, so mitochondrial dysfunction often causes poor focus, memory lapses, and mental fatigue.
- Poor muscle endurance – Mitochondria are concentrated in muscles, and when they underperform, even climbing stairs can feel overwhelming.
- Unrefreshing sleep – Even with 8–9 hours in bed, patients with mitochondrial dysfunction often wake up feeling like they never rested.
This pattern is one reason why chronic fatigue syndrome (CFS/ME) and post-viral fatigue are often linked to underlying mitochondrial issues.
Functional Medicine and Mitochondrial Health
At Sheen Vein & Cosmetics, we take a functional medicine approach to fatigue. Rather than just prescribing a stimulant or sleep aid, we ask: Why aren’t your mitochondria producing enough energy?
Our evaluation often includes:
- Advanced nutrient testing to check for deficiencies in magnesium, B12, carnitine, and CoQ10.
- Inflammation markers to uncover hidden immune activity that may be suppressing mitochondria.
- Hormone testing for thyroid, adrenal, and testosterone function.
- Toxin exposure evaluation, since mold, heavy metals, and chemicals can all impair mitochondrial health.
By identifying root causes, we can target mitochondrial repair rather than just masking fatigue.
Supporting Mitochondrial Function
Patients are often relieved to learn that mitochondria can be supported and, in many cases, repaired. Our strategies include:
- Nutritional Support
- CoQ10 and PQQ for mitochondrial energy pathways
- Magnesium to activate ATP
- B vitamins to drive the Krebs cycle
- Carnitine to shuttle fatty acids into mitochondria
- Reducing Oxidative Stress
Antioxidants like vitamin C, glutathione, and alpha-lipoic acid help protect mitochondria from free radical damage. - Lifestyle Changes
- Intermittent fasting and exercise can stimulate mitochondrial biogenesis—the creation of new, healthy mitochondria.
- Stress management lowers cortisol and reduces mitochondrial strain.
- Regenerative Therapies
We also offer advanced options such as red light therapy with PEMF, which directly stimulates mitochondrial energy production and supports tissue repair.
The Bigger Picture
Chronic fatigue isn’t just “in your head.” If you’ve been told your labs are normal yet you still feel exhausted, the issue may be happening at the cellular level. By addressing mitochondrial dysfunction, many patients experience not only improved energy but also better mood, sharper cognition, and greater resilience.
Take Back Your Energy
At Sheen Vein & Cosmetics in St. Louis, we specialize in uncovering the hidden drivers of fatigue through a root-cause functional medicine approach. If you’re tired of being tired, it may be time to evaluate your mitochondrial health and restore your body’s ability to generate energy.
👉 Learn more about our functional medicine services
👉 Schedule your consultation today