The Connection Between Depression and Gut Health: What Your Microbiome Has to Do with Your Mood
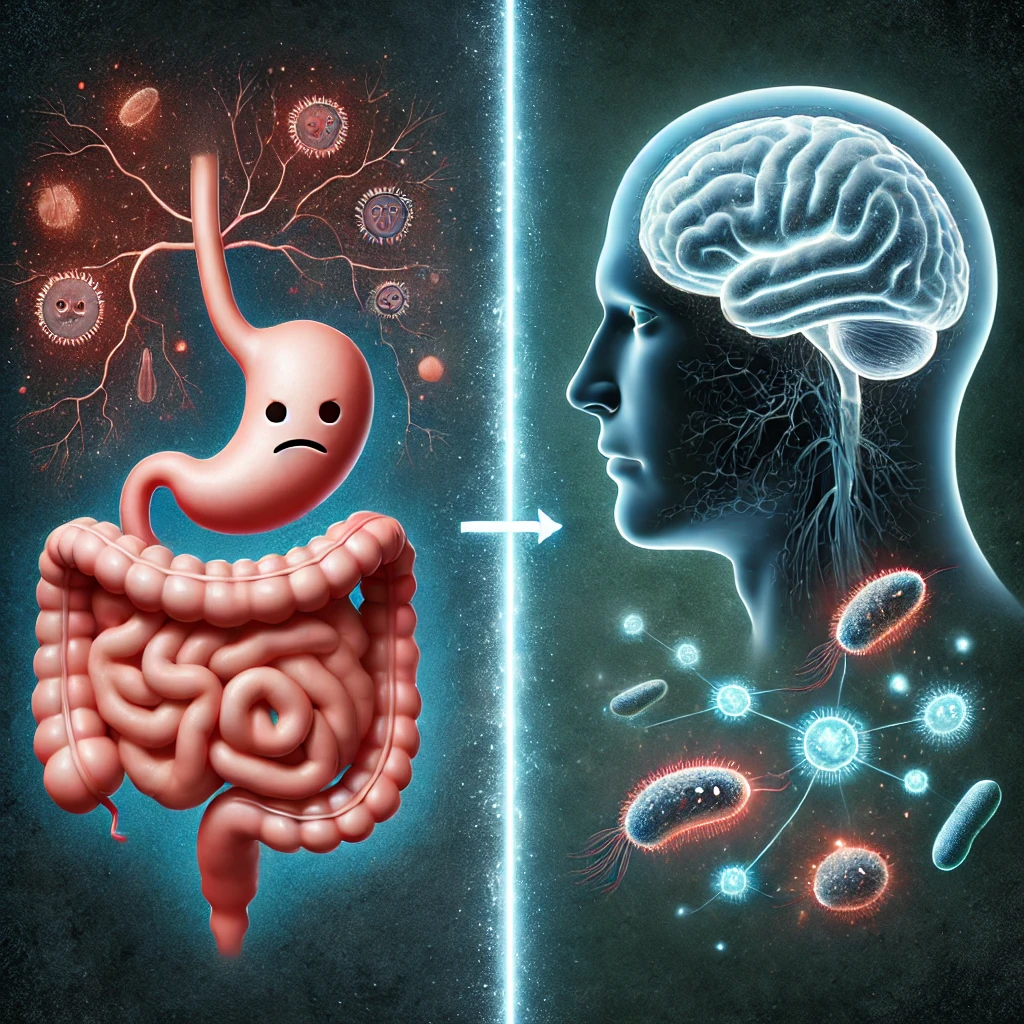
The Connection Between Depression and Gut Health
How Healing the Gut Can Help Heal the Mind
If you’ve been struggling with depression, anxiety, or emotional overwhelm, you’ve probably heard suggestions like “try therapy,” “get more sunlight,” or “consider medication.” But what if one of the most overlooked contributors to your mood lives in your gut?
Research is revealing an intimate link between gut health and brain function, and it’s changing the way we understand mental health conditions like depression.
This link is called the gut-brain axis—and it may hold the key to unlocking lasting mood resilience and emotional balance.
So, what exactly is the connection between depression and gut health? And how can you support your microbiome to feel better, from the inside out?
The Gut-Brain Axis: Your Second Brain
Your gastrointestinal tract isn’t just for digestion—it’s also home to a complex network of neurons known as the enteric nervous system, sometimes called your “second brain.” It produces many of the same neurotransmitters (brain chemicals) as your central nervous system, including:
- Serotonin – regulates mood, sleep, and appetite
- Dopamine – involved in pleasure, motivation, and reward
- GABA – helps calm the nervous system
- Norepinephrine – modulates alertness and energy
In fact, over 90% of your body’s serotonin is made in the gut, not the brain.
Your gut and brain constantly communicate via the vagus nerve, as well as through chemical messengers, immune pathways, and the gut microbiota (the ecosystem of trillions of microbes living in your digestive tract).
This two-way communication is what scientists refer to as the gut-brain axis.
How Gut Health Affects Depression
When your gut is healthy and balanced, your brain benefits. But when your gut is imbalanced—due to dysbiosis, leaky gut, or inflammation—your mood can suffer significantly.
Here are six key ways your gut impacts your mental health:
✅ 1. Your Microbiome Helps Regulate Neurotransmitters
Certain gut bacteria are responsible for producing or modulating neurotransmitters like:
- Lactobacillus and Bifidobacterium – influence GABA production
- Enterococcus and Streptococcus species – may help with serotonin synthesis
When your microbiome is out of balance, it can reduce these beneficial compounds, leaving you more prone to low mood, anxiety, and emotional dysregulation.
✅ 2. Inflammation in the Gut Can Lead to Inflammation in the Brain
Chronic gut inflammation can trigger systemic inflammation, including in the brain. This is sometimes called neuroinflammation, and it’s been linked to:
- Major depressive disorder
- Brain fog and cognitive decline
- Sleep disturbances
- Low motivation and energy
Gut imbalances often lead to increased intestinal permeability (aka “leaky gut”), allowing toxins like lipopolysaccharide (LPS) to enter the bloodstream and trigger inflammation and immune activation in the brain.
✅ 3. Your Gut Impacts the HPA Axis (Stress Response System)
The hypothalamic-pituitary-adrenal (HPA) axis regulates your body’s stress response, including cortisol release. A compromised gut can dysregulate this axis, leading to:
- Heightened stress sensitivity
- Poor cortisol rhythm
- Exhaustion and burnout
This gut-driven dysregulation may explain why people with IBS or leaky gut often experience heightened anxiety and depressive symptoms.
✅ 4. Your Gut Bacteria Affect Tryptophan Metabolism
Tryptophan is an amino acid precursor to serotonin. Certain gut microbes help convert tryptophan into serotonin, while others may shunt it into inflammatory pathways like kynurenine, which has been linked to depressive symptoms.
A healthy gut helps favor mood-supporting pathways. An imbalanced gut may do the opposite.
✅ 5. Gut Health Affects Nutrient Absorption for Mental Health
Your gut is where you absorb key nutrients needed to make neurotransmitters, including:
- Vitamin B12 and folate – needed for methylation and serotonin production
- Magnesium – supports GABA, stress resilience, and calm
- Zinc – involved in neurotransmitter balance and brain repair
- Omega-3s – reduce inflammation and support brain cell function
Gut inflammation or dysbiosis can impair absorption of these nutrients, making it harder for your brain to maintain emotional stability.
✅ 6. Probiotic Strains Can Improve Mood
Clinical research shows that certain probiotic strains can directly impact emotional health:
- Lactobacillus helveticus and Bifidobacterium longum have been shown in studies to reduce anxiety and depression symptoms
- These are often referred to as psychobiotics—probiotics that positively influence the mind
These findings reinforce the idea that nurturing your gut can support your mental health—without always needing pharmaceutical intervention.
Common Signs of Gut-Driven Depression
If you have depression along with the following symptoms, your gut health may be playing a role:
- Bloating, gas, or food intolerances
- Constipation or loose stools
- Sugar cravings
- Brain fog or poor concentration
- Fatigue despite sleeping
- Skin issues like eczema or acne
- A history of antibiotic overuse
How to Improve Gut Health for Better Mood
Functional medicine takes a root-cause approach to depression by addressing the gut-brain axis. Here’s where to start:
✅ 1. Cut Out Inflammatory Triggers
- Eliminate processed foods, added sugar, and artificial additives
- Identify and remove food sensitivities (e.g., gluten, dairy, corn)
- Avoid excess alcohol or NSAIDs, which damage the gut lining
✅ 2. Rebuild the Gut Lining
- Use L-glutamine, zinc carnosine, and collagen to repair leaky gut
- Consider medical-grade probiotics and prebiotics
- Add bone broth, aloe vera, or slippery elm to soothe gut inflammation
✅ 3. Feed the Right Bacteria
- Increase fiber from veggies, fruits, chia seeds, and legumes
- Add fermented foods like sauerkraut, kefir, kimchi, or miso
- Rotate your produce to feed a diverse microbiome
✅ 4. Manage Stress with Nervous System Support
- Practice deep breathing, meditation, yoga, or grounding
- Get outside daily—sunlight and nature improve both gut flora and mood
- Try adaptogens like ashwagandha or Rhodiola if approved by your provider
✅ 5. Consider Functional Testing
Comprehensive gut tests (like GI-MAP or Genova GI Effects) can assess:
- Gut bacteria balance
- Inflammation and immune markers
- Leaky gut indicators (zonulin, calprotectin)
- Yeast or parasite overgrowth
Personalized treatment based on test results leads to better outcomes for depression and gut healing.
Final Thoughts: Heal the Gut, Heal the Mind
The connection between depression and gut health is no longer just a theory—it’s an evolving field of science known as psychoneurogastroenterology. And it’s changing lives.
Your gut is more than your digestive system—it’s a command center that influences your brain, mood, and emotional resilience.
If you’re struggling with depression and haven’t addressed your gut, now is the time. Healing your microbiome may be one of the most powerful steps you can take to improve your mood—naturally, holistically, and sustainably.
At Sheen Vein and Cosmetics, we help uncover the root causes of mental health struggles through gut testing, microbiome rebalancing, nutritional therapy, and functional medicine protocols tailored to you.
📞 Ready to explore how your gut health may be affecting your mood? Schedule a consultation with our functional team today.
W