Understanding Chronic Venous Insufficiency: Why Your Legs May Hurt, Swell, or Feel Heavy
Introduction
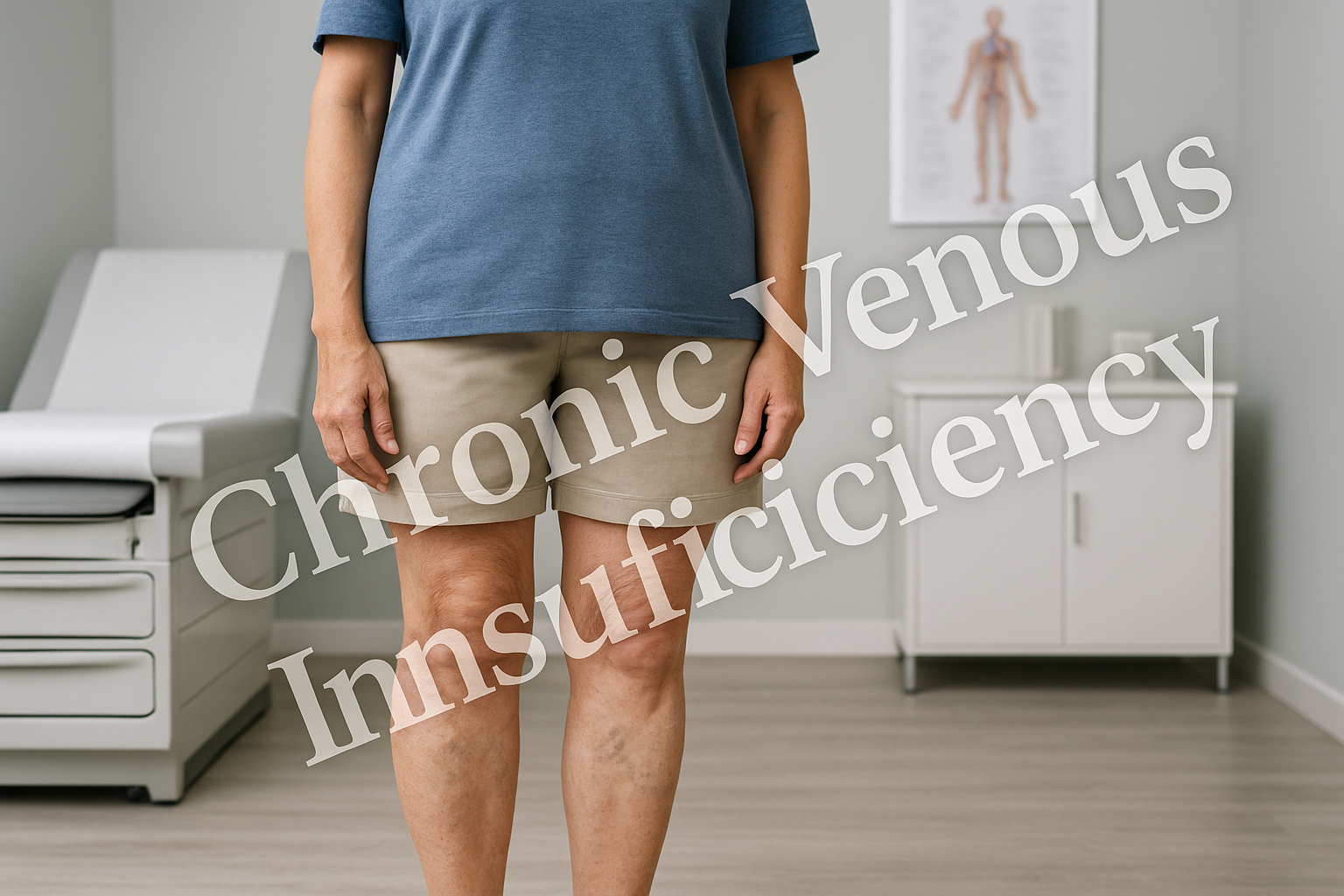
If you’ve been dealing with leg swelling, aching, or varicose veins, you may be experiencing more than just a cosmetic concern. These symptoms often point to an underlying condition called chronic venous insufficiency (CVI).
As a physician, I see this condition frequently — and too often it goes unrecognized until it causes significant discomfort or complications. CVI is not just about how your legs look; it’s about how your veins are functioning.
In this article, I’ll explain what chronic venous insufficiency is, why it happens, how we diagnose it, and the treatment options available to improve both symptoms and long-term vascular health.
What Is Chronic Venous Insufficiency?
Chronic venous insufficiency occurs when the veins in your legs cannot efficiently return blood back to the heart. Normally, the veins have one-way valves that prevent blood from flowing backward. In CVI, these valves weaken or fail, causing blood to pool in the legs.
Over time, this leads to increased venous pressure, swelling, skin changes, and in severe cases, ulcers.
CVI affects an estimated 20–40% of adults, making it one of the most common vascular conditions.
Symptoms of Chronic Venous Insufficiency
The symptoms of CVI vary from mild discomfort to advanced skin changes. Many patients dismiss the early signs as “just being on my feet too long.” Recognizing them early is important.
Common Symptoms
- Leg swelling (especially around the ankles)
- Aching, throbbing, or heaviness in the legs
- Burning, cramping, or restless legs at night
- Itching or tingling in the legs
- Visible varicose veins or spider veins
- Skin discoloration around the ankles (brownish or reddish patches)
- Slow-healing wounds or ulcers on the lower leg
Symptoms often worsen after standing or sitting for long periods and improve when the legs are elevated.
Risk Factors for Chronic Venous Insufficiency
Several factors increase the risk of CVI:
- Age – risk increases as valves weaken with time
- Gender – women are more affected, partly due to hormonal influences and pregnancy
- Family history – genetics play a significant role
- Pregnancy – increased blood volume and pressure on pelvic veins
- Obesity – excess weight strains the venous system
- Prolonged standing or sitting – common in certain occupations (nurses, teachers, cashiers, office workers)
- History of blood clots (DVT) – damage to deep veins raises risk
- Smoking – weakens blood vessels and reduces circulation
How We Diagnose Chronic Venous Insufficiency
Diagnosis begins with a careful clinical evaluation. As a physician, I combine a thorough history with physical examination and specialized imaging.
Steps in Diagnosis:
- History & symptom review – identifying swelling, leg heaviness, varicose veins, or ulcer history.
- Physical exam – looking for visible varicose veins, skin changes, or swelling.
- Venous duplex ultrasound – the gold standard test. It uses sound waves to check blood flow, valve function, and rule out blood clots.
- Clinical classification (CEAP system) – physicians classify venous disease based on severity, from mild varicose veins (C2) to active ulcers (C6).
Why Chronic Venous Insufficiency Matters
CVI is more than an annoyance — left untreated, it can progress and cause serious complications.
- Varicose veins can worsen, leading to bleeding or clotting within the vein.
- Edema (swelling) can cause skin breakdown.
- Stasis dermatitis – chronic inflammation leads to skin thickening and discoloration.
- Venous ulcers – painful, slow-healing wounds near the ankles that can become infected.
- Increased risk of deep vein thrombosis (DVT).
Addressing venous insufficiency early helps prevent these complications and greatly improves comfort and quality of life.
Treatment Options for Chronic Venous Insufficiency
The good news is that CVI can be effectively managed. Treatment depends on severity but usually involves a combination of lifestyle changes, compression therapy, and minimally invasive procedures.
1. Conservative Measures
- Compression stockings – improve circulation and reduce swelling.
- Leg elevation – raising legs above heart level helps drain pooled blood.
- Exercise – walking strengthens calf muscles, which act as a “pump” for venous return.
- Weight management – reduces pressure on veins.
2. Medications
While no pill “cures” venous insufficiency, certain medications can help:
- Venoactive drugs (such as micronized flavonoids) may improve circulation.
- Anti-inflammatories or antibiotics may be needed if skin complications occur.
3. Minimally Invasive Procedures
Modern vein treatments are highly effective and performed in-office with little downtime. Options include:
- Endovenous laser ablation (EVLA) – uses laser energy to close faulty veins.
- Radiofrequency ablation (RFA) – similar to EVLA, but uses radiofrequency heat.
- Ultrasound-guided foam sclerotherapy – a medicated foam seals off varicose veins.
- Visually guided sclerotherapy – injecting surface reticular veins and spider veins.
These procedures reroute blood flow into healthier veins, reducing pressure and improving symptoms.
Lifestyle and Functional Medicine Support
In addition to medical treatments, supporting vascular health through lifestyle and nutrition plays an important role.
- Diet rich in antioxidants (berries, green leafy vegetables, citrus bioflavonoids) supports blood vessel integrity.
- Hydration helps maintain circulation.
- Avoiding long periods of sitting/standing by moving every 30–60 minutes.
- Targeted supplements (under clinician guidance) such as horse chestnut extract or pycnogenol may improve venous tone.
Prevention: Protecting Your Vein Health
While you can’t change your genetics or age, there are practical steps to lower your risk or slow progression of CVI:
- Wear compression stockings during long flights or work shifts.
- Maintain a healthy weight.
- Stay physically active, especially walking.
- Elevate your legs when resting.
- Avoid smoking, which damages blood vessels.
Practical Steps if You Suspect CVI
If you’re experiencing symptoms such as leg swelling, heaviness, or visible varicose veins, don’t ignore them. Here’s what to do:
- Schedule an evaluation with a vein specialist or vascular physician.
- Request a venous ultrasound to assess valve function.
- Begin conservative measures right away (compression, elevation, movement).
- Discuss minimally invasive treatment options if symptoms persist.
Conclusion
Chronic venous insufficiency is a progressive but highly treatable condition. Too often, patients dismiss their symptoms as “just getting older” or “bad circulation,” but the reality is that CVI has clear causes, diagnostic tools, and effective treatments.
With the right care, patients can reduce leg pain and swelling, improve mobility, and prevent serious complications like ulcers.
If you’re struggling with leg heaviness, swelling, or varicose veins, know that help is available. A thorough evaluation and personalized treatment plan can restore your leg health and your quality of life.